Zero Provider Counties: The Stark Reality of Maternity Care Deserts in Mississippi
This post is the first of a three-part series examining the state of maternal care in Mississippi.
Your water breaks unexpectedly at 35 weeks pregnant. You have no reliable transportation and a limited support system. It’s 3:00 AM. Will the neighbor answer the door? Your contractions don’t seem to be the “real thing,” but maybe they are. Your obstetrician and hospital are over 90 miles away…
If asked to pinpoint the location matching the described scenario, some would guess a low-and-middle-income country, a remote village perhaps, not counties deemed maternity care deserts that are quickly covering the United States.
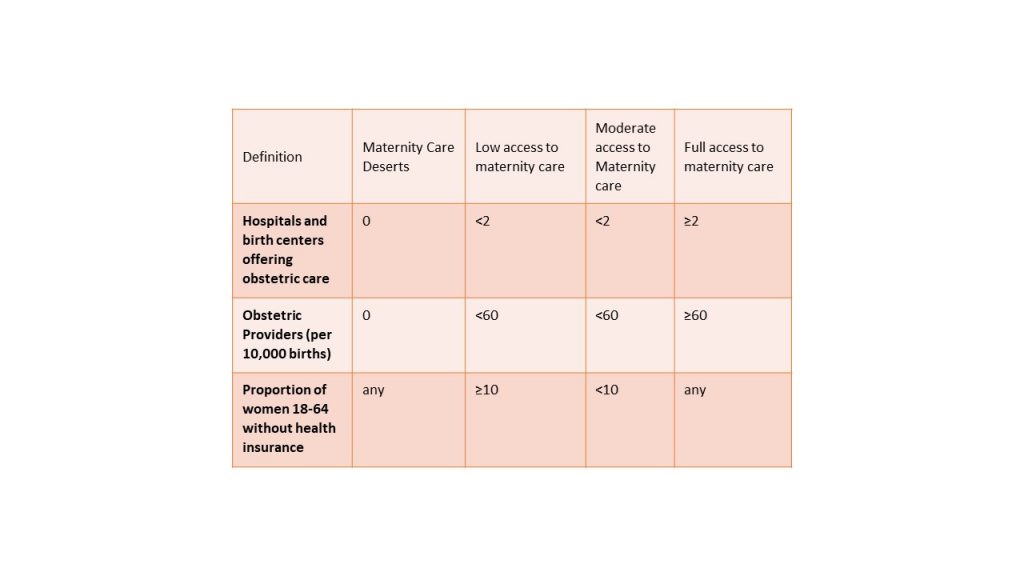
According to a report by the March of Dimes, “maternity care deserts are any county without a hospital or birth center offering obstetric care and without any obstetric providers.” There are 1,095 maternity care deserts within the United States. From a quantitative perspective, the chart below outlines the differences between maternity care deserts and areas with low, moderate, and full access to maternity care.
Within the U.S., more than 2.2 million women of childbearing age live in maternity care deserts and an additional 4.8 million women of childbearing age live in counties with limited access to maternity care. Maternity care deserts are associated with higher rates of poverty and lower median household income than counties with moderate or full access to maternity care.
A study found that the risk of death during pregnancy and up to one-year postpartum was significantly elevated among women residing in maternity care deserts, compared with women in areas with moderate to full access to maternity care. This is further exacerbated by racial inequities across non-Hispanic Black and Native American populations, versus white non-Hispanic women.

The Outlook for Mississippi
Mississippi, a largely rural population with 54% of the population living in rural areas, has greater than 50% of its healthcare providers practicing in urban settings designating 82 counties as medically underserved. In the state of Mississippi, 45 of the state’s 82 counties are considered either maternity care deserts or have low access to maternity care.
This causes pregnant women to seek care from an OBGYN outside of their county for both prenatal care and delivery services. This impacts Black and indigenous populations disproportionately, with 76.2% of birth parents living in maternity care deserts being from non-White races (23.9% Black, 51.3% Native American, 19.1% Hispanic, 11.9% Native Hawaiian/Pacific Islander, 5.6% Asian).
Geographic accessibility to adequate health care providers and services, both in terms of distance and time traveled, has been recognized by experts and policymakers alike as a key dimension of access, pivotal to maternity care. According to the March of Dimes, in Mississippi, 13.6% of women receive inadequate prenatal care during their pregnancy.
About 20% of Mississippi women had less than adequate prenatal care, and racial disparities in prenatal care utilization were observed. Black women delayed prenatal care, received too few visits, and were more likely to have either “inadequate prenatal care” or “no care” compared to white women. Women who delay or receive no prenatal care are more likely to deliver a low-birthweight infant or have a preterm birth compared to women receiving early care. Inadequate prenatal care is associated with an increased risk for neonatal death. Moreover, maternal mortality is significantly higher among rural populations, demonstrated by CDC data from 2015 with a national metropolitan maternal mortality rate of 18.2 deaths per 100,000 live births compared with rural maternal mortality rate of 29.4 deaths per 100,000 live births.
In part two of this series, we will explore deepening health inequities in Mississippi that contribute to this issue affecting Black women and the role that health coverage plays in addressing this crisis. Subscribe to our newsletter so you don’t miss any updates.


Sorry, the comment form is closed at this time.