Postpartum Depression Among Black Mothers
Epidemiological Overview
According to the Pregnancy Risk Assessment Monitoring System, postpartum depression impacts one in eight women residing in the United States (Depression Among Women, 2020). Although the prevalence of postpartum depression varies greatly by state, Mississippi has the highest rate with 23.5% of women reporting symptoms. The incidence for postpartum depression is approximately 600,000 annual cases (4 million annual live births as the denominator).
Prevalence of postpartum depression is impacted by socio-demographic factors, especially in terms of race with 18.2% of Black non-Hispanic women, compared with 12% of Hispanic women, and 11.4% of White non-Hispanic women. Other socio-demographic factors that impact prevalence of postpartum depression include:
Age
- 22.2% of women <19
- 17.8% of women ages 20-24
- 11.9% of women 25-24
- 10.8% of women >35
Marital Status
- 16.9% of unmarried women
- 11% of married women
Education
- 17.8% of women with <12 years education
- 11.2% of women with >12 years education
Health Insurance Status
- 10.1% of women with private insurance
- 13.2% of uninsured women
- 17.2% of women covered by Medicaid
Black women are impacted disproportionately, not because of biological causes, but rather due to systemic racism that increases health inequities, worsening maternal health outcomes.

Risk & Protective Factors
Black women are more likely to have depression prior or during pregnancy, which is the most prominent indicator of onset of postpartum depression. Among women with self-reported depression during pregnancy, 34% developed postpartum depression. Additionally, infant gestation age and mortality impact likelihood of postpartum depression, with a correlation between traumatic birth experience and onset of postpartum depression.
Infant mortality among Black mothers is experienced at 11.7 deaths per 1,000 live births compared with the national average of six deaths per 1,000 live births. Approximately 48.7% of mothers who experienced an infant death developed symptoms of postpartum depression and 17.1% of women who had a preterm birth developed postpartum depression symptoms.
Other associated risk factors for Black women include lack of social support, demographic factors, history of depression, lack of self-efficacy, lack of access to care, and perceptions of trust with medical providers. Protective factors that decrease risk of postpartum depression and/or increase likelihood of timely diagnosis and treatment include demographic factors, insurance, education, marital status, infant health status, as well as history of mental health conditions. Black women who do not have a previous mental health condition are less susceptible to developing postpartum depression.
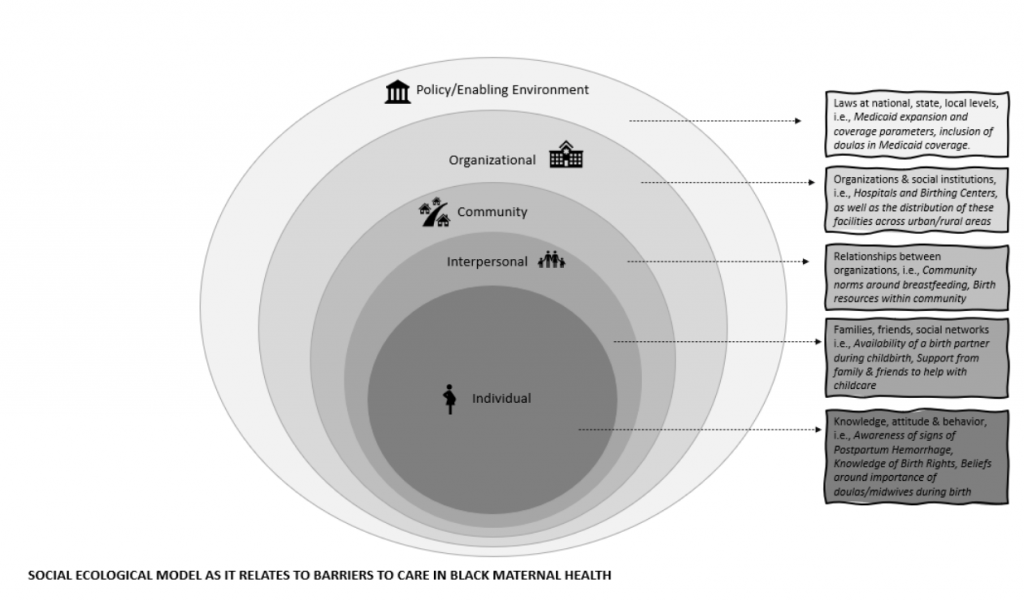
Social Ecology of Postpartum Depression
The social ecological framework of postpartum depression demonstrates multiple levels of risks that influence postpartum depression in the black community. At the individual level, knowledge of the symptoms of postpartum depression coupled with self-efficacy to seek care, influence diagnosis and treatment. Initiating mental health care for postpartum depression is lower for Black women than White women. This was demonstrated in a study of 29,601 women in New Jersey’s Medicaid program where only 4% of black women with postpartum depression symptoms sought care compared with 9% of White women.
Self-efficacy in care seeking behavior is influenced, especially in the Black community, by stigmas. Many communities do not accept mental health care and medication-based treatment. For instance, Black mothers with postpartum depression are less likely to accept prescription medication and mental health counseling in comparison to White counterparts. Social determinants to health, especially in terms of access, availability, and quality of care are also critical factors that influence the timely detection and treatment of postpartum depression in Black communities.
Developmental Timing of Postpartum Depression
Symptoms of postpartum depression can be confused with the “baby blues” during the first two weeks postpartum, whereas postpartum depression lasts for prolonged periods. Detecting, diagnosing, and treating depression during the prenatal period is the most malleable point of intervention to ensure the mother is monitored for signs of postpartum depression. Failing to diagnose and/or treat postpartum depression has adverse effects for mother and child, including long-term effects for cognitive, emotional, and behavioral development.
Black women are at greater risk for non-detection of mental health conditions compared to White women, which can be attributed to care seeking behaviors. The American College of Obstetricians and Gynecologists, as well as The American Academy of Pediatrics, urge obstetric care providers and pediatricians to include screening for depression in routine visits from the prenatal to postpartum period, including during well-child visits.
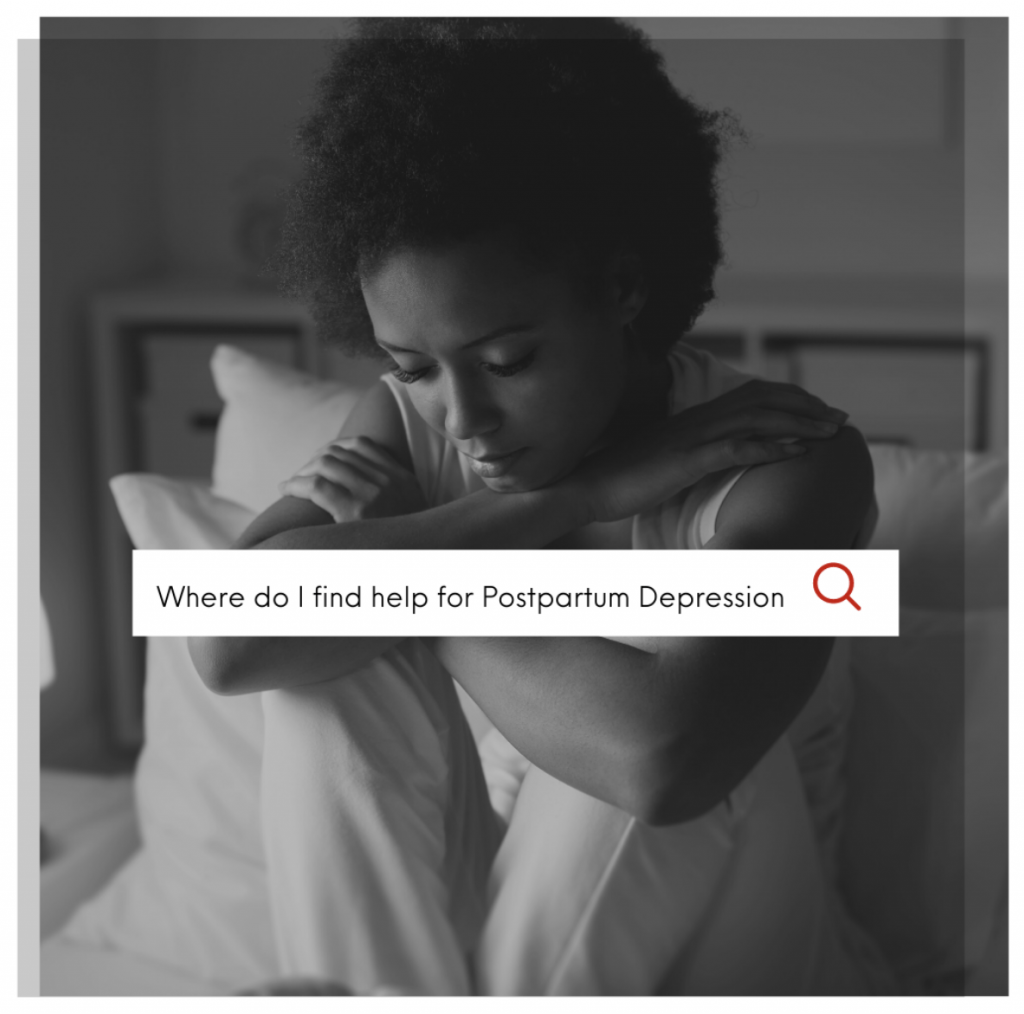
Seeking Care
If you are experiencing symptoms of postpartum depression, do not feel ashamed to seek care. The Substance Abuse and Mental Health Services Administration (SAMHSA) offers a free, confidential, treatment referral service. Call 1-800-662-HELP (4357). Your mental health is equally important to your physical health. It’s okay to not be okay.


Sorry, the comment form is closed at this time.