Zero Provider Counties: Deepening Health Inequities
This post is part two of a three-part series examining the state of maternal care in Mississippi. To read part one, click here.
Health Coverage and Medicaid Expansion
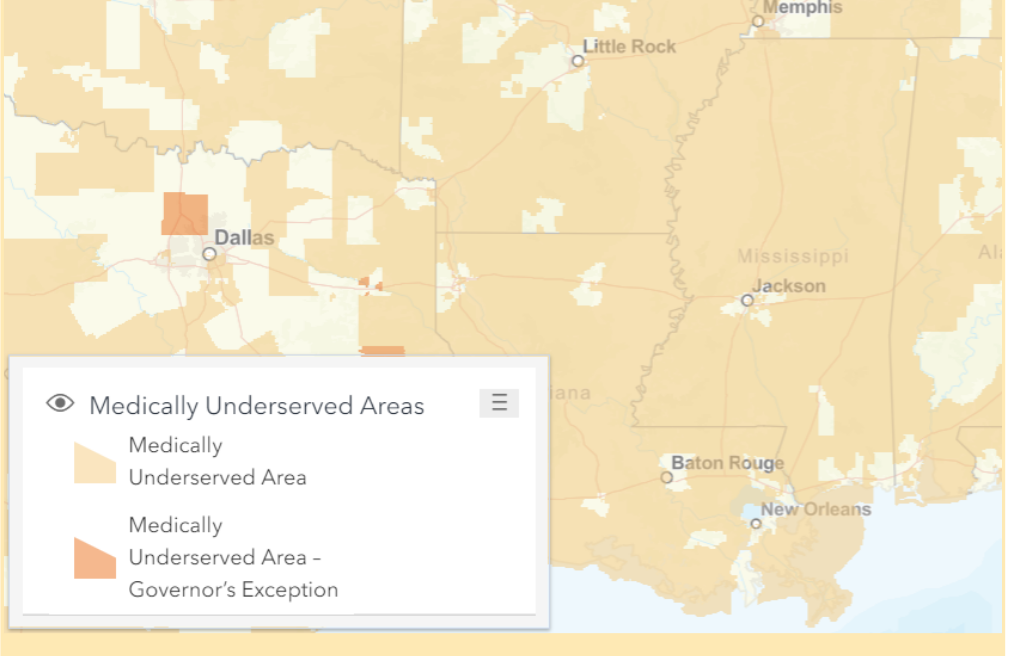
Health coverage in Mississippi is lacking with an uninsured population 14.5% greater than the national average, leaving 351,794 nonelderly Mississippians (ages 0-64) uninsured. Mississippi voted to not expand Medicaid, under the Affordable Care Act, which aimed to provide coverage to non-elderly adults 138% below the federal poverty line. If expanded, Medicaid would have benefited an additional 170,000+ uninsured adults as of 2018.
The lack of access to care in terms of distribution of health facilities and providers, coupled with affordability, left 26.5% of residents 18 and older without a personal health care provider in 2019. Additionally, 17.2% of residents age 18 and older did not see a doctor in 2019 due to the factor of cost. Medicaid expansion leads to better health coverage for reproductive age women, earlier initiation of prenatal care, better care prior to pregnancy, and lower rates of maternal mortality. A study found that Medicaid expansion was associated with lower rates of maternal mortality, reflecting 1.6 fewer maternal deaths per 100,000 women.
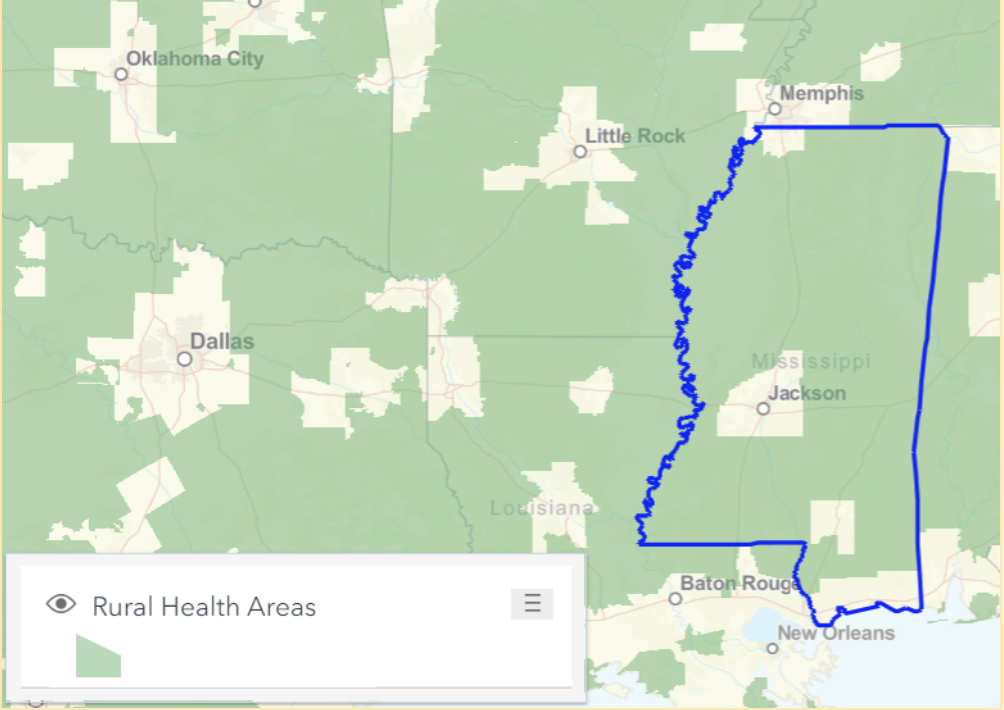
As of 2018, 41.3% of Mississippians were 200% below the Federal Poverty Level. Beyond the obvious statement that maternity care deserts lack appropriate infrastructure and density of healthcare workers, women of reproductive age are often living in poverty, suffer from racial disparities, and are likely underinsured or uninsured. Health centers in rural areas serve double the percentage of uninsured patients, compared with the national average (22% vs. 11%) and 65% of uninsured rural women had a hospital birth, a much lower rate than the almost 100% for both Medicaid and privately insured, rural women.
Mississippi Medicaid reports that 46% of covered women who delivered babies in 2019 did not have a postpartum visit at all, while the national average number of visits is 1.1 visits per woman. Mississippi is one of twelve states with the highest rates of uninsured women of childbearing age. Although Medicaid’s relatively high eligibility covers delivery, lower-income women are at significant risk of being uninsured in critical months before pregnancy, during the prenatal period, and after delivery.
Deepening Health Inequities
Inequities in Mississippi among expectant mothers in areas deemed maternity care deserts, are attributable to restrictive policies limiting health coverage and access to sexual and reproductive health services, the effects of systemic racism, and poverty. The collision of these factors increases risk of poor maternal health outcomes like maternal mortality and morbidity, infant mortality, and poor birth outcomes like preterm births.
Mississippi’s conservative nature hinders the rights of Black women of reproductive age living in rural settings. Uninsured and underinsured women do not have the financial resources to fulfill their health needs, let alone the needs of a child in utero. Women are left with difficult decisions to forgo monthly prenatal care and to schedule elective cesarean sections in fear they will not be able to make it to the hospital prior to childbirth.
The inequities that Black women face in maternity care deserts demonstrates the importance of intersectionality in not only considering the geographic location of a childbearing woman, but also insurance coverage and race. The interplay of these factors deepens inequity, while increasing biases this population faces when striving to seek, reach, and receive quality maternal healthcare. Furthermore, lack of health facilities and obstetric providers in maternity care deserts demonstrates the principles of distributive justice and structural injustice, due to the imbalanced distribution of critical health resources and insurance. This also includes the laws and policies reinforced by government systems in Mississippi that create a disadvantage that is both unfair and unjust.
In the final installment of this series, we will propose a solution to address the issues we’ve explored. Subscribe to our newsletter, The Equity Report, using the form below for more news and research around maternal health.

No Comments